108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

COPD 与支气管扩张共存:COPD 患者主要肺动脉与主动脉直径比(PA:A)较高的危险因素
Authors Dou S, Zheng C, Ji X, Wang W, Xie M, Cui L, Xiao W
Received 5 November 2017
Accepted for publication 17 January 2018
Published 26 February 2018 Volume 2018:13 Pages 675—681
DOI https://doi.org/10.2147/COPD.S156126
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Charles Downs
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Chunxue Bai
Background: Pulmonary vascular disease, especially pulmonary hypertension, is
an important complication of COPD. Bronchiectasis is considered not only a
comorbidity of COPD, but also a risk factor for vascular diseases. The main
pulmonary artery to aorta diameter ratio (PA:A ratio) has been found to be a
reliable indicator of pulmonary vascular disease. It is hypothesized that the
co-existence of COPD and bronchiectasis may be associated with relative
pulmonary artery enlargement (PA:A ratio >1).
Methods: This retrospective study enrolled COPD patients from
2012 through 2016. Demographic and clinical data were collected. Bhalla score
was used to determine the severity of bronchiectasis. Patient characteristics
were analyzed in two ways: the high (PA:A >1) and low (PA:A ≤1) ratio
groups; and COPD with and without bronchiectasis groups. Logistic regression
analysis was used to assess risk factors for high PA:A ratios.
Results: In this study, 480 COPD patients were included, of
whom 168 had radiographic bronchiectasis. Patients with pulmonary artery enlargement
presented with poorer nutrition (albumin, 35.6±5.1 vs 38.3±4.9, P <0.001), lower oxygen partial
pressure (74.4±34.5 vs 81.3±25.4, P <0.001), more
severe airflow obstruction (FEV1.0, 0.9±0.5 vs 1.1±0.6, P =0.004), and a higher frequency
of bronchiectasis (60% vs 28.8%, P <0.001) than
patients in the low ratio group. Patients with both COPD and bronchiectasis had
higher levels of systemic inflammation (erythrocyte sedimentation rate, P <0.001 and fibrinogen, P =0.006) and PA:A ratios (P <0.001). A higher PA:A ratio
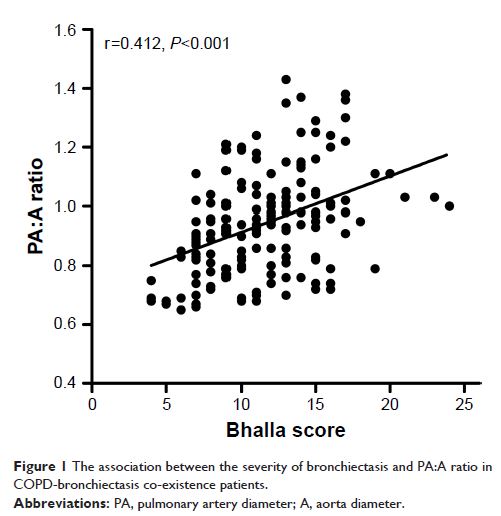
was significantly closely correlated with a higher Bhalla score (r=0.412, P <0.001). Patients with both
COPD and bronchiectasis with high ratios presented higher levels of NT-proBNP (P <0.001) and systolic pulmonary
artery pressure (P <0.001). Multiple logistic
analyses have indicated that bronchiectasis is an independent risk factor for
high PA:A ratios in COPD patients (OR =3.707; 95% CI =1.888–7.278; P <0.001).
Conclusion: Bronchiectasis in COPD has been demonstrated to be
independently associated with relative pulmonary artery enlargement.
Keywords: COPD,
bronchiectasis, main pulmonary artery to aorta diameter ratio, pulmonary
vascular disease, CT