108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

食管鳞状细胞癌食管切除术后继发性淋巴结转移患者放疗疗效及预后的影响因素
Authors Zhou SB, Guo XW, Gu L, Ji SJ
Received 26 July 2017
Accepted for publication 5 December 2017
Published 2 February 2018 Volume 2018:10 Pages 217—225
DOI https://doi.org/10.2147/CMAR.S147324
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Akshita Wason
Peer reviewer comments 3
Editor who approved publication: Dr Antonella D'Anneo
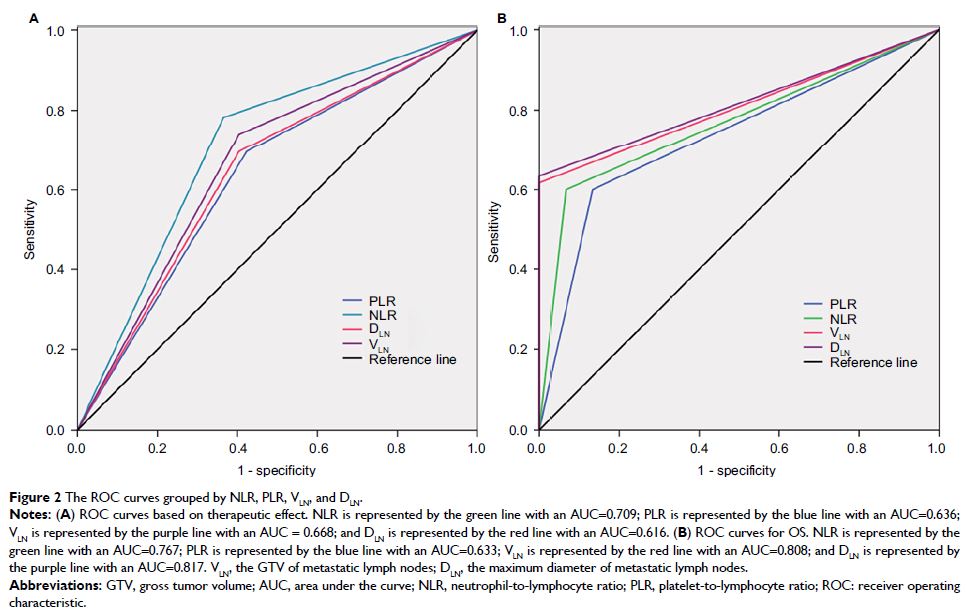
Background: The purpose of this study was to clarify whether pretreatment
tumor burden-related index, including the gross tumor volume (GTV) of
metastatic lymph nodes (VLN) and maximum
diameter of metastatic lymph nodes (DLN), and
inflammatory markers, consisting of neutrophil-to-lymphocyte ratio (NLR) and
platelet-to-lymphocyte ratio (PLR), are useful for assessing the therapeutic
effects and prognosis with secondary lymph node metastasis (LNM) receiving
chemoradiotherapy (CRT) or radiotherapy (RT) alone after resection of
esophageal squamous cell carcinoma (ESCC).
Patients and
methods: A total of 119 patients with
secondary LNM after resection of ESCC were recruited and received curative RT
only or CRT. The enrolled patients were grouped according to the median values
of NLR, PLR, VLN, and DLN. The relationship between the responsiveness to
treatment and these markers was analyzed by logistic analysis. The Kaplan–Meier
method and log-rank test were adopted to calculate and compare the overall
survival (OS) rates with these markers. The Cox models were used to carry out
multivariate analyses.
Results: Univariate logistic regression analysis showed that the responses
to treatment were highly associated with treatment method (P =0.011), NLR (P =0.000), PLR (P =0.003), VLN (P =0.000), and DLN (P =0.000). Next,
multivariate logistic regression analysis showed that therapeutic method
(hazard ratio [HR]=1.225, P =0.032), NLR
(HR=2.697, P =0.019), and VLN (HR=4.607, P =0.034)
were independent risk factors for tumor response. Additionally, Kaplan–Meier
survival analysis of this cohort revealed that NLR (Χ 2=27.298, P =0.000), PLR (Χ 2=16.719, P =0.000), VLN (Χ 2=48.823, P =0.000), DLN (Χ 2=40.724, P =0.000), and
treatment methods (Χ 2=18.454, P =0.018) were
significantly associated with OS. Furthermore, multivariate analysis was
performed, and the results showed that therapeutic method (HR=1.223, P =0.048), NLR (HR=2.000, P =0.018), VLN (HR=2.379, P =0.020),
and DLN (HR=2.901, P =0.002)
were considered independent prognostic factors for OS.
Conclusion: This study found that NLR and VLN were
promising as predictive markers for therapeutic effects, and NLR combined with
VLN and with DLN might be
useful biomarkers in predicting outcomes in patients with secondary LNM
receiving CRT or single RT after esophagectomy.
Keywords: esophageal carcinoma, tumor volume, hematological markers,
therapeutic response, prognostic factor, chemoradiotherapy