108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

预测北京地区老年男性原发性骨质疏松症的三种预测工具的比较:横断面研究
Authors Zhang X, Lin J, Yang Y, Wu H, Li Y, Yang X, Fei Q
Received 6 July 2017
Accepted for publication 8 December 2017
Published 2 February 2018 Volume 2018:13 Pages 201—209
DOI https://doi.org/10.2147/CIA.S145741
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 3
Editor who approved publication: Dr Wu
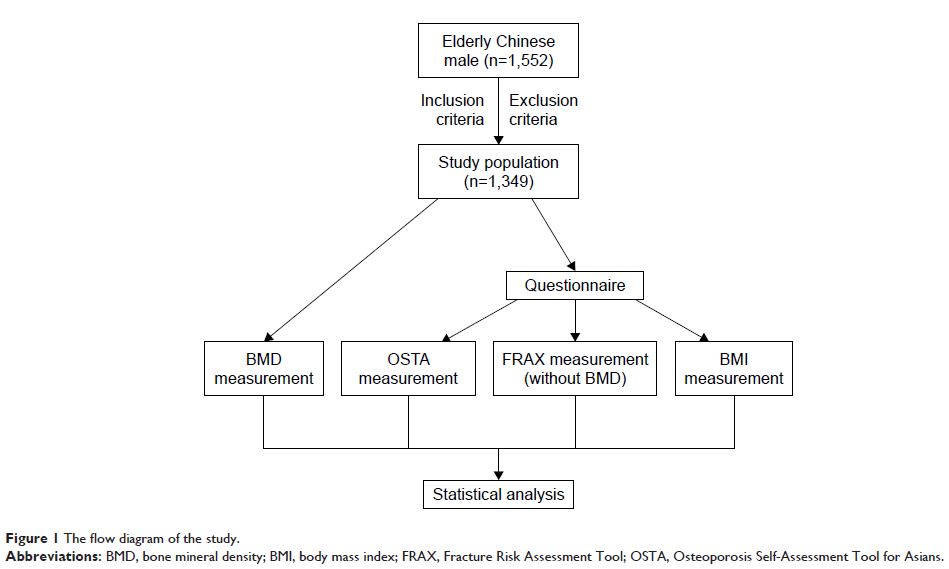
Purpose: In this cross-sectional study, three clinical tools, the
Osteoporosis Self-Assessment Tool for Asians (OSTA), Fracture Risk Assessment
Tool (FRAX) without bone mineral density (BMD), and body mass index (BMI), for
predicting primary osteoporosis (OP) were compared and ideal thresholds for
omission of screening BMD were proposed in a community-dwelling elderly Han
Beijing male population.
Patients and
methods: A total of 1,349 community-dwelling
elderly Han Beijing males aged ≥50 years were enrolled in this study.
All subjects completed a questionnaire and measured BMD by dual-energy X-ray
absorptiometry (DXA). Osteoporosis was defined as a T-score of -2.5 SD or lower
than that of the average young adult in different diagnostic criteria (lumbar
spine [L1–L4], femoral neck, total hip, worst hip, and World Health
Organization [WHO]). FRAX without BMD, OSTA, and BMI were assessed for
predicting OP by receiver operating characteristic (ROC) curves. Sensitivity,
specificity, and areas under the ROC curves (AUCs) were determined. Ideal
thresholds for omission of screening BMD were proposed.
Results: The prevalence of OP ranged from 1.8% to 12.8% according to
different diagnostic criteria. This study showed that the BMI has highest
discriminating ability. The AUC of FRAX without BMD ranged from 0.536 to 0.630,
which suggested limiting predictive value for identifying OP in elderly Beijing
male. The AUCs of BMI (0.801–0.880) were slightly better than OSTA
(0.722–0.874) in predicting OP at all sites. The AUC of BMI to identify OP in
worst hip was 0.824, yielding a sensitivity of 84.8% and a specificity of
64.4%. 40% of participants on BMD measurements saved only 0.1%–2.7% missed OP.
Compared to OSTA and FRAX without BMD, the BMI got the best predictive value
for OP.
Conclusion: BMI may be a simple and effective tool for identifying OP in the
elderly male population in Beijing to omit BMD screening reasonably.
Keywords: male, osteoporosis, Osteoporosis Self-Assessment Tool for Asians,
OSTA, Fracture Risk Assessment Tool, FRAX, body mass index, BMI