108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

宫颈癌中 PD-1/PD-L1 路径与 DNA 错配修复的关系及其临床意义
Authors Feng YC, Ji WL, Yue N, Huang YC, Ma XM
Received 21 September 2017
Accepted for publication 1 December 2017
Published 18 January 2018 Volume 2018:10 Pages 105—113
DOI https://doi.org/10.2147/CMAR.S152232
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Akshita Wason
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Background: According to recent clinical observations, deficient DNA mismatch
repair (dMMR) is capable of improving antitumor effects of the PD-1/PD-L1
pathway, suggesting that dMMR may act as a prognostic indicator of PD-1/PD-L1
antibody drugs. In this study, we examined the dMMR and PD-1/PD-L1 expression,
as well as explored the correlation of dMMR status with PD-1/PD-L1 expression
in cervical cancer patients, in order to optimize cervical cancer patient
selection for PD-1/PD-L1 antibody drug treatment, which is helpful to avoid
adverse effects and keep costs manageable.
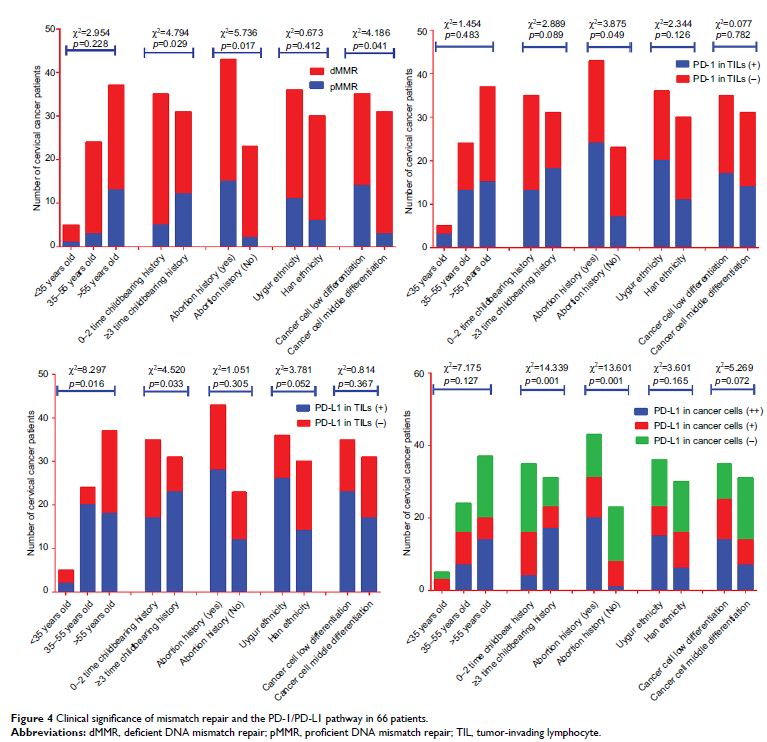
Methods: Sixty-six tissue samples from patients with
squamous cell carcinoma were collected, and data of their clinical
characteristics were also gathered. Based on these samples, the expression
levels of MLH1, MSH2, and PD-L1 in cancer cells were tested by
immunohistochemical assay (IHC). Moreover, PD-1/PD-L1 expression in
tumor-invading lymphocytes (TILs) was detected by IHC as well. Six
single-nucleotide-repeat markers of microsatellite instability (MSI), including
NR-27, MONO-27, BAT-25, NR-24, NR-21, and BAT-26, were tested by capillary
electrophoresis sequencer analysis. According to expression of MLH1, MSH2 and
the MSI test, all 66 cases were divided into dMMR or proficient DNA mismatch
repair (pMMR) groups. The comparisons of dMMR and PD-L1 in cancer cells and of
PD-1/PD-L1 in TILs were conducted categorized by age, childbearing history,
history of abortion, ethnicity, and cancer cell differentiation subgroup.
Furthermore, PD-L1 levels in cancer cells and PD-1/PD-L1 in TILs were analyzed
and compared in both dMMR and pMMR subgroups.
Results: Of the patient samples, 25.8% were associated
with dMMR. PD-L1 in cancer cells, PD-L1 in TILs, and PD-1 in TILs took up
59.1%, 47.0%, and 60.6%, respectively. The data indicated that both dMMR and
PD-L1 overexpression resulted from lower cancer differentiation, more
incidences of childbearing, and a history of abortion. Abortion could
significantly increase PD-1 expression levels in TILs. Additionally, more
incidence of childbearing or older age (35–55 years) was able to upregulate
PD-L1 expression in TILs. Statistical difference of PD-L1 in cancer cells could
be observed between dMMR and pMMR subgroups. In the dMMR group, PD-L1 in cancer
cells and PD-1 in TILs had no correlation (r s=0.161, p =0.537), but in
the pMMR group, they had good correlation (r s=0.645, p <0.001).
Conclusion: According to prior studies and our own
experiments, PD-L1 in both cancer cells and TILs and PD-1 in TILs are widely
observed in cervical cancer patients, indicating that there may be potential to
apply PD-1/PD-L1 antibody drugs in cervical cancer. dMMR patients are
associated with higher PD-L1 expression compared with pMMR ones, which
suggested that PD-1/PD-L1 antibody drugs may work well in dMMR cervical cancer
patients. Moreover, in patients with more incidences of childbearing or
abortion, dMMR may be a molecular detection target for clinical application of
PD-1/PD-L1 antibody drugs.
Keywords: programmed cell
death 1, programmed cell death 1 ligand 1, DNA mismatch repair system, cervical
cancer