108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

全身性免疫炎症指标作为有用的预后指标,用于预测新辅助化疗治疗的进展期胃癌患者的生存率
Authors Chen L, Yan Y, Zhu L, Cong X, Li S, Song S, Song H, Xue Y
Received 6 September 2017
Accepted for publication 31 October 2017
Published 14 December 2017 Volume 2017:9 Pages 849—867
DOI https://doi.org/10.2147/CMAR.S151026
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Akshita Wason
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
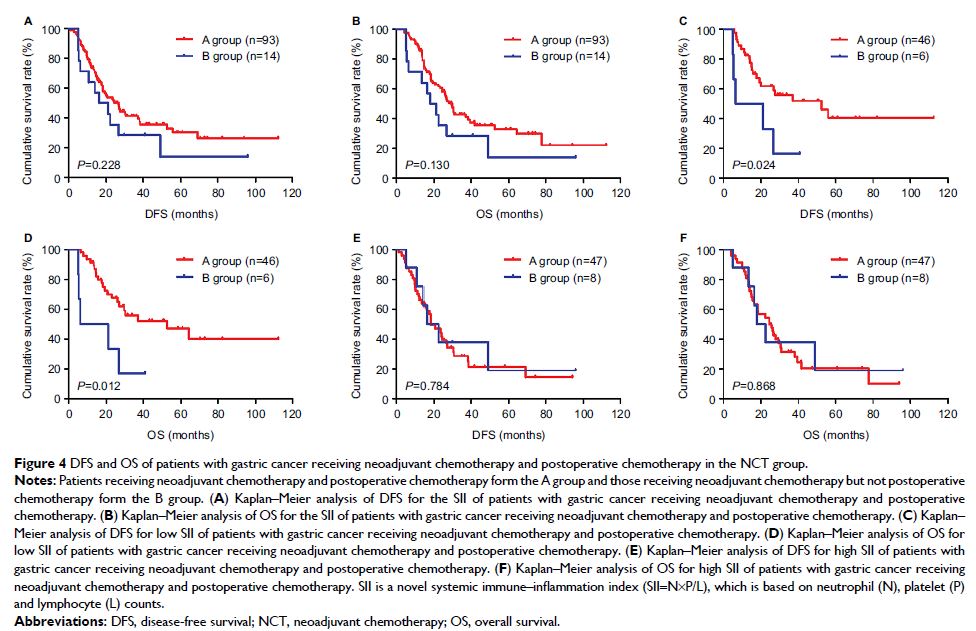
Background and
objective: A novel systemic immune–inflammation
index named SII (SII=N×P/L), which is based on neutrophil (N), platelet (P) and
lymphocyte (L) counts, has emerged and reflects comprehensively the balance of
host inflammatory and immune status. We aimed to evaluate the potential
prognostic significance of SII in patients with advanced gastric cancer who
received neoadjuvant chemotherapy.
Subjects and
methods: The retrospective analysis included
data from 107 patients with advanced gastric cancer undergoing neoadjuvant
chemotherapy and 185 patients with pathology-proven gastric cancer. The optimal
cutoff value of SII by receiver operating characteristic curve stratified
patients into low SII (<600×109/L) and high SII (SII ≥600×109/L) groups. The clinical outcomes of disease-free survival (DFS) and
overall survival (OS) were calculated by Kaplan–Meier survival curves and
compared using log-rank test. Univariate and multivariate Cox proportional
hazards regression models were used to analyze the prognostic value of SII.
Results: The results indicated that SII had prognostic significance using
the cutoff value of 600×109/L on DFS and OS in univariate and multivariate Cox regression survival
analyses. Low SII was associated with prolonged DFS and OS, and the mean DFS
and OS for patients with low SII were longer than for those with high SII
(57.22 vs 41.56 months and 62.25 vs 45.60 months, respectively). Furthermore,
we found that patients with low SII had better 1-, 3- and 5-year rates of DFS
and OS than those with high SII. In addition, patients with low SII were likely
to receive DFS and OS benefits from neoadjuvant chemotherapy and postoperative
chemotherapy.
Conclusion: SII may qualify as a noninvasive, cost-effective, convenient and
reproducible prognostic indicator for patients with advanced gastric cancer
undergoing neoadjuvant chemotherapy. It may help clinicians to identify those
patients who will benefit from treatment strategy decisions.
Keywords: neoadjuvant chemotherapy, gastric cancer, systemic
immune–inflammation index, SII, prognosis