108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Improved spirometric detection of small airway narrowing: concavity in the expiratory flow–volume curve in people aged over 40 years
Authors Johns DP, Das A, Toelle BG, Abramson MJ, Marks GB, Wood-Baker R, Walters EH
Received 29 August 2017
Accepted for publication 15 November 2017
Published 13 December 2017 Volume 2017:12 Pages 3567—3577
DOI https://doi.org/10.2147/COPD.S150280
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Charles Downs
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Background and
objective: We have explored whether assessing
the degree of concavity in the descending limb of the maximum expiratory
flow–volume curve enhanced spirometric detection of early small airway disease.
Methods: We used spirometry records from 890 individuals
aged ≥40 years (mean 59 years), recruited for the Burden of Obstructive Lung
Disease Australia study. Central and peripheral concavity indices were
developed from forced expired flows at 50% and 75% of the forced vital
capacity, respectively, using an ideal line joining peak flow to zero flow.
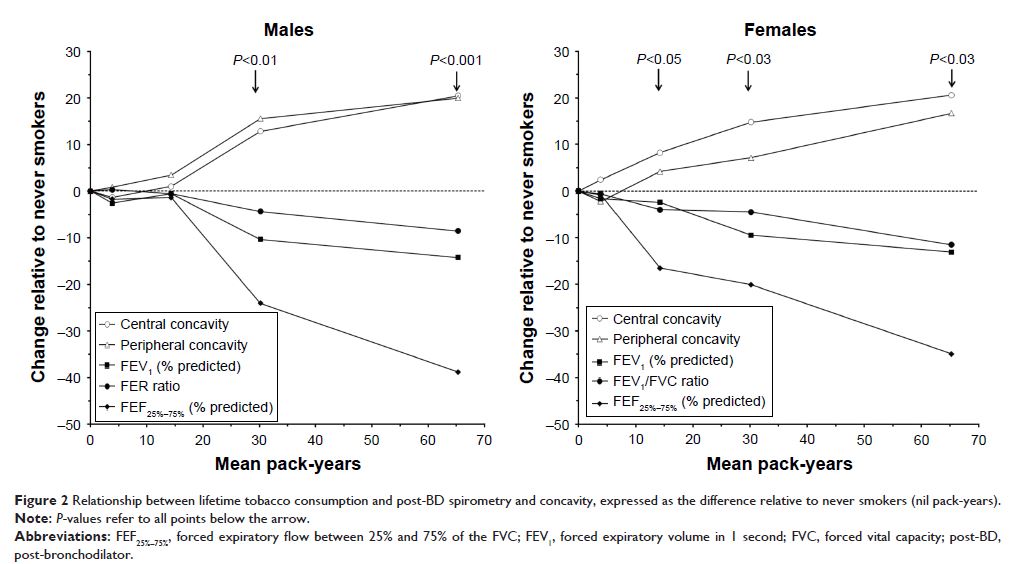
Results: From the 268 subjects classified as normal never
smokers, mean values for post-bronchodilator central concavity were 18.6% in
males and 9.1% in females and those for peripheral concavity were 50.5% in
males and 52.4% in females. There were moderately strong correlations between
concavity and forced expired ratio (forced expiratory volume in
1 second/forced vital capacity) and mid-flow rate (forced expiratory flow
between 25% and 75% of the FVC [FEF25%–75%]; r=-0.70
to -0.79). The additional number of individuals detected as abnormal using the
concavity indices was substantial, especially compared with FEF25%–75%, where it was approximately doubled.
Concavity was more specific for symptoms.
Conclusion: The inclusion of these concavity measures in the
routine reports of spirometry would add information on small airway obstruction
at no extra cost, time, or effort.
Keywords: early airway
disease, airflow obstruction, COPD