108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

肿瘤沉积是同时行结直肠癌同时性肝转移切除的病患的不良预后指标
Authors Lin Q, Wei Y, Ren L, Zhong Y, Qin C, Zheng P, Xu P, Zhu D, Ji M, Xu J
Published Date January 2015 Volume 2015:8 Pages 233—240
DOI http://dx.doi.org/10.2147/OTT.S71414
Received 19 July 2014, Accepted 4 September 2014, Published 22 January 2015
Background: Tumor deposits are one of the important
influencing factors among the different editions of Tumor, Node, Metastasis classification.
Incidence and prognosis of tumor deposits in stage I, II, and III colorectal
cancer patients has been explored. The aim of this study was to determine the
prognostic value of tumor deposits in stage IV colorectal cancer patients who
underwent simultaneous resection for synchronous colorectal liver metastases
(SCRLM).
Methods: Clinicopathological
and outcome data of 146 consecutive SCRLM patients who underwent simultaneous
R0 resection between July 2003 and July 2013 were collected from our prospectively
established SCRLM database. The prognostic value of tumor deposits was
evaluated by Kaplan–Meier and Cox regression analysis.
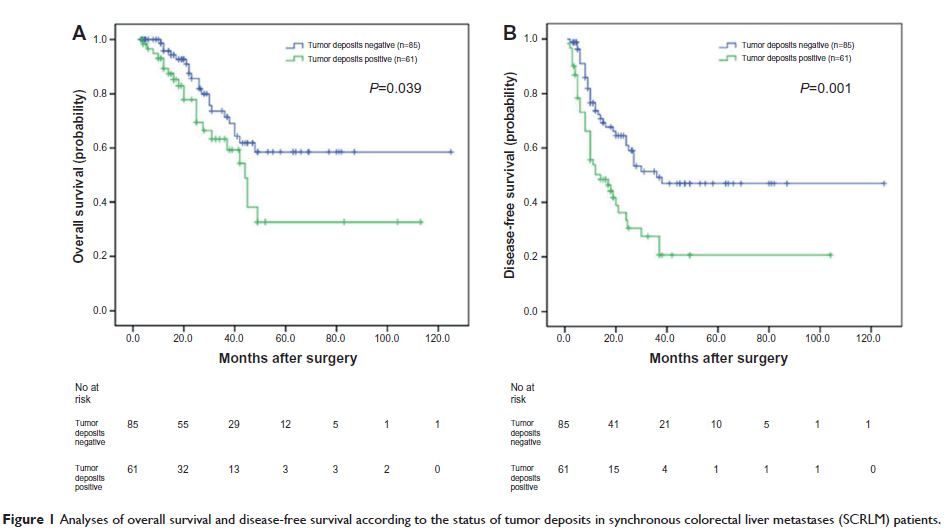
Results: Tumor deposits were
detected in 41.8% (61/146) of these SCRLM patients. Tumor deposits were
significantly correlated with lymph node metastasis and nerve invasion of the
primary tumors (P =0.002, P =0.041; respectively). The
Kaplan–Meier survival analysis revealed that the overall survival (OS) and
disease-free survival (DFS) of SCRLM patients with tumor deposits were
significantly poorer than those with no tumor deposits (P =0.039, P =0.001; respectively). And with
multivariate analysis, we found that positive tumor deposits were significantly
associated with shorter DFS independent of lymph node status (P =0.002). Subgroup analysis found
that of the 57 SCRLM patients with negative lymph node status, the OS and DFS
of patients with positive tumor deposits were significantly shorter than those
with negative tumor deposits (P =0.002 and P =0.031, respectively). Of the 89 patients
with positive lymph node status, the OS of patients with tumor deposits was not
significantly different than those without tumor deposits (P =0.965); however, the DFS of
patients with tumor deposits was significantly shorter than those with no tumor
deposits (P =0.034).
Conclusion: Tumor deposits may
be an independent adverse prognostic factor in SCRLM patients who underwent
simultaneous R0 resection.
Keywords: tumor deposits,
synchronous colorectal liver metastases, prognostic factors