108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

活检标本中 CD8+ 淋巴细胞密度及循环淋巴细胞比值可预测直肠癌放化疗的病理完全反应
Authors Xiao BY, Peng JH, Zhang RX, Xu J, Wang YC, Fang YJ, Lin JZ, Pan ZZ, Wu XJ
Received 1 September 2017
Accepted for publication 12 October 2017
Published 27 November 2017 Volume 2017:9 Pages 701—708
DOI https://doi.org/10.2147/CMAR.S150622
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
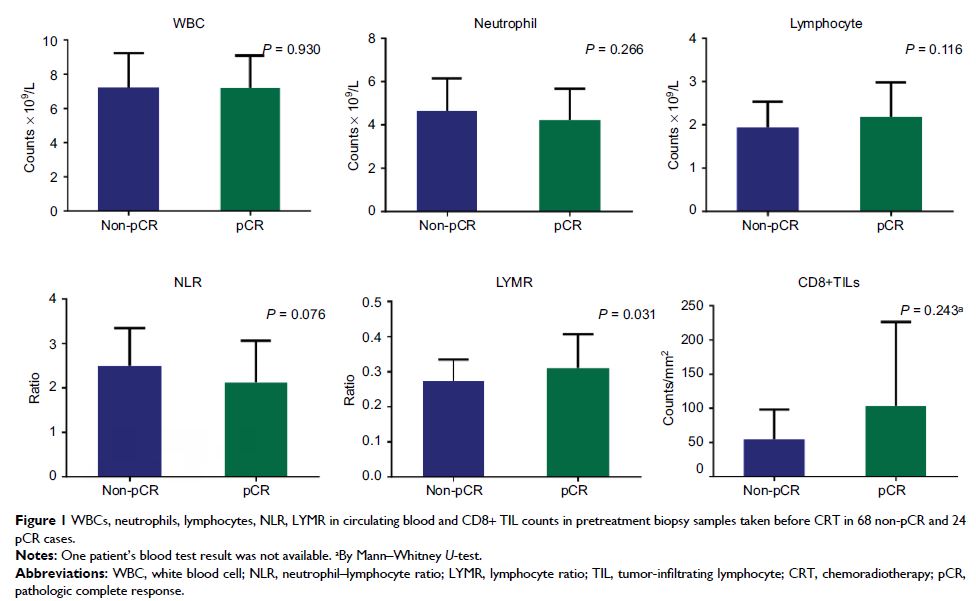
Objectives: The systemic status and local immune status, as determined by the
neutrophil–lymphocyte ratio (NLR) or the lymphocyte ratio (LYMR) and
tumor-infiltrating lymphocyte (TIL) count, respectively, have been suggested as
predictors of the tumor response to neoadjuvant chemoradiotherapy (nCRT) in
rectal cancer, although the utility of these measures remains controversial. We
aimed to investigate the values of the LYMR, NLR and TIL count and their
combinations (TIL–LYMR/TIL–NLR) in predicting pathologic complete response
(pCR) after nCRT.
Patients and methods: Pretreatment biopsy samples and data from the blood
tests of 92 patients with rectal cancer who underwent curative resection after
nCRT were retrospectively obtained. CD8+ TILs were immunostained using an
antibody against CD8. The density of CD8+ TILs was recorded as the number of
CD8+ T cells per square millimeter, and the results were classified as either
“high” or “low”. The LYMR and NLR were calculated using pretreatment blood test
data and categorized into either “high” or “low” groups. TIL–LYMR was graded as
“low,” “mid” or “high” when neither, one or both the CD8+ TIL count and LYMR
were “high,” respectively. TIL–NLR was graded similarly. The associations
between TILs and LYMR, NLR and their combinations (TIL–LYMR/TIL–NLR) were
evaluated.
Results: pCR was significantly associated with a high LYMR, a
low NLR and increased chemotherapy cycles (P =0.039, P =0.043 and P =0.015, respectively), but not
with the CD8+ TIL count or carcinoembryonic antigen (CEA) level (P =0.100 and P =0.590, respectively).
Additionally, 40% of patients with high LYMR and 40.7% with low NLR achieved
pCR, whereas only 19.7% with low LYMR and 20.3% with high NLR did so. When the
combinations were assessed, TIL–LYMR showed a positive correlation with pCR (P =0.038), while no association
between TIL–NLR and pCR was found (P =0.916). In
multivariate analysis, TIL–LYMR remained an independent predictor of pCR (odds
ratio [OR]=1.833, 95% confidence interval [CI]=1.069–3.142, P =0.028).
Conclusion: High LYMR, low NLR and high TIL–LYMR at baseline
are predictive of pCR to nCRT for patients with rectal cancer. These parameters
may help identify pCR patients and provide additional information for
therapeutic decision-making.
Keywords: chemoradiotherapy,
rectal cancer, pathologic complete response, tumor-infiltrating lymphocytes,
lymphocyte ratio, neutrophil–lymphocyte ratio