108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

戒烟影响 COPD 的自然病程
Authors Bai J, Chen X, Liu S, Yu L, Xu JF
Received 30 August 2017
Accepted for publication 4 October 2017
Published 16 November 2017 Volume 2017:12 Pages 3323—3328
DOI https://doi.org/10.2147/COPD.S150243
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Chunxue Bai
Background: Cigarette
smoking is the most commonly encountered and readily identifiable risk factor
for COPD. However, it is not clear which quantitative factors related to
smoking influence the prognosis of COPD patients.
Methods: A total of 204 patients with a long-term history of smoking were
enrolled into this study and followed up for 5 years. Patients were divided
into “death” or “survival” groups based on follow-up results and
“quitting-smoking” or “continuing-smoking” groups based on whether they gave up
smoking.
Results: Patients in the death group had a longer smoking time, lower
prevalence of quitting smoking, later onset of COPD symptoms, older age at
quitting smoking, lower forced expiratory volume in one second (FEV1) % predicted, and lower ratio of FEV1/forced vital capacity. Age, age at quitting smoking, and FEV1% predicted were independently associated with mortality from COPD.
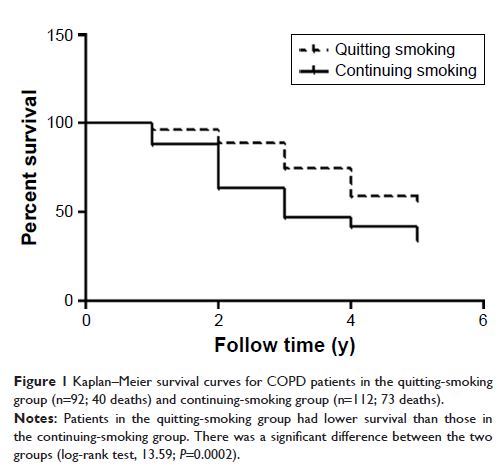
Compared to the continuing-smoking group, the quitting-smoking group had a
lower mortality rate, longer course of COPD, earlier onset of COPD symptoms,
and lower residual volume percent predicted. During the 5-year follow-up, 113
deaths were recorded (quitting-smoking group: n=92; 40 deaths;
continuing-smoking group: n=112; 73 deaths). The mortality risk remained significantly
higher in the continuing-smoking group than the quitting-smoking group
(log-rank test, 13.59; P =0.0002).
Conclusion: Smoking time may be related to the mortality rate from COPD. Smoking
cessation has the greatest capacity to influence the natural history of COPD.
Keywords: chronic obstructive pulmonary disease, cigarette smoking, smoking
cessation