108985
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

尼妥珠单抗联合同步放化疗有利于晚期鼻咽癌患者
Authors Li Z, Li Y, Yan S, Fu J, Zhou Q, Huang X, Shen L
Received 10 May 2017
Accepted for publication 20 September 2017
Published 14 November 2017 Volume 2017:10 Pages 5445—5458
DOI https://doi.org/10.2147/OTT.S141538
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Akshita Wason
Peer reviewer comments 2
Editor who approved publication: Dr Faris Farassati
Background: The
potential benefits and possible risks associated with combined nimotuzumab and
concurrent chemoradiotherapy in patients with advanced nasopharyngeal carcinoma
(NPC) have yet to be determined.
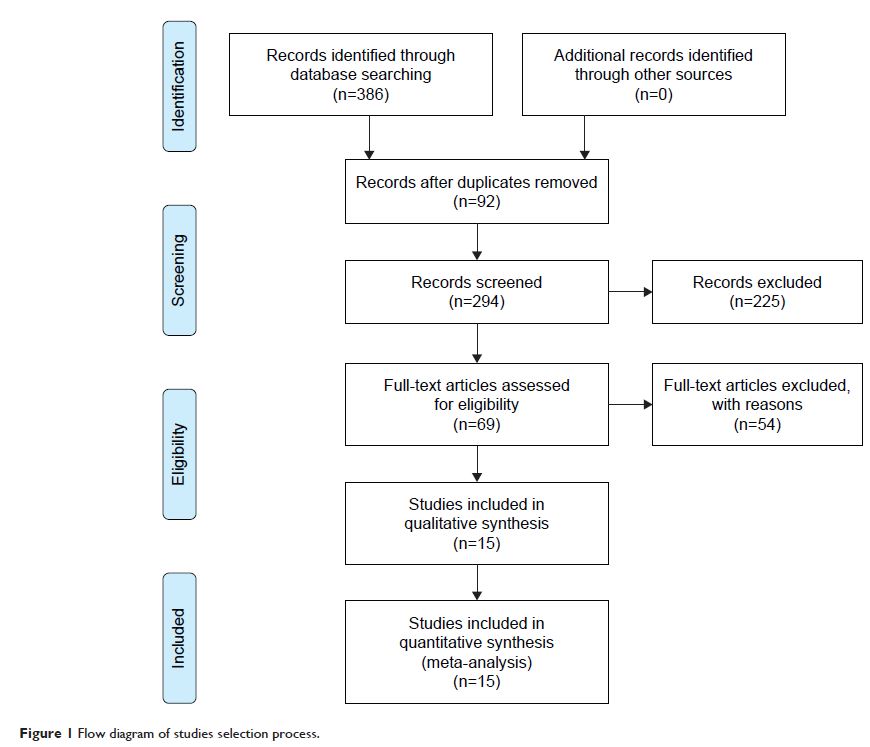
Methods: The databases PubMed, Web of Science, China National Knowledge
Infrastructure, and Wanfang were systematically searched through February 2017
for studies comparing combined nimotuzumab and chemoradiotherapy versus
chemoradiotherapy alone in the treatment of NPC. Primary outcomes were complete
and partial responses, and the secondary outcome was adverse reactions. The
random-effect model was used to pool relative risks (RRs) and 95% confidence
intervals (CIs).
Results: Nine randomized control trials and six cohort studies were included in
the final analysis (n=1,015 patients). Compared with chemoradiotherapy alone,
chemoradiotherapy combined with nimotuzumab was associated with an increased
response rate (RR =1.11, 95% CI: 1.01–1.22). Combined treatment further
reduced the occurrence rate of erythropenia (RR =0.11, 95% CI: 0.05–0.28)
and neutropenia (RR =0.12, 95% CI: 0.05–0.27). The differences in the
rates of other complications were not significant.
Conclusion: Nimotuzumab combined with concurrent chemoradiotherapy is more
effective in patients with advanced NPC than chemoradiotherapy alone. Patients
receiving combination therapy did not have a higher rate of adverse reactions.
Nimotuzumab can thus be recommended as an adjunct therapy in patients with
advanced NPC.
Keywords: randomized controlled trial, cohort studies, nasopharyngeal carcinoma,
relative risk, radiotherapy, chemoradiotherapy