109229
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Efficiency of spinal anesthesia versus general anesthesia for lumbar spinal surgery: a retrospective analysis of 544 patients
Authors Pierce JT, Kositratna G, Attiah MA, Kallan MJ, Koenigsberg R, Syre P, Wyler D, Marcotte PJ, Kofke WA, Welch WC
Received 6 May 2017
Accepted for publication 18 July 2017
Published 10 October 2017 Volume 2017:10 Pages 91—98
DOI https://doi.org/10.2147/LRA.S141233
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 2
Editor who approved publication: Dr Stefan Wirz
Background: Previous studies have shown varying results in selected outcomes
when directly comparing spinal anesthesia to general in lumbar surgery. Some
studies have shown reduced surgical time, postoperative pain, time in the
postanesthesia care unit (PACU), incidence of urinary retention, postoperative
nausea, and more favorable cost-effectiveness with spinal anesthesia. Despite
these results, the current literature has also shown contradictory results in
between-group comparisons.
Materials and
methods: A retrospective analysis was
performed by querying the electronic medical record database for surgeries
performed by a single surgeon between 2007 and 2011 using procedural codes
63030 for diskectomy and 63047 for laminectomy: 544 lumbar laminectomy and
diskectomy surgeries were identified, with 183 undergoing general anesthesia
and 361 undergoing spinal anesthesia (SA). Linear and multivariate regression
analyses were performed to identify differences in blood loss, operative time,
time from entering the operating room (OR) until incision, time from bandage
placement to exiting the OR, total anesthesia time, PACU time, and total
hospital stay. Secondary outcomes of interest included incidence of
postoperative spinal hematoma and death, incidence of paraparesis, plegia,
post-dural puncture headache, and paresthesia, among the SA patients.
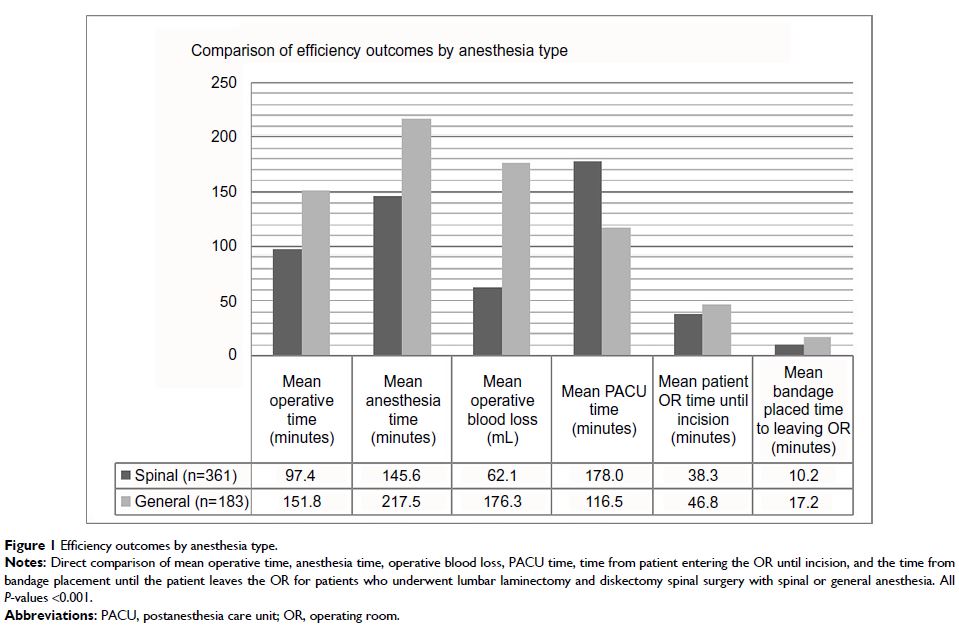
Results: SA was associated with significantly lower operative time, blood
loss, total anesthesia time, time from entering the OR until incision, time
from bandage placement until exiting the OR, and total duration of hospital
stay, but a longer stay in the PACU. The SA group experienced one spinal
hematoma, which was evacuated without any long-term neurological deficits, and
neither group experienced a death. The SA group had no episodes of paraparesis
or plegia, post-dural puncture headaches, or episodes of persistent
postoperative paresthesia or weakness.
Conclusion: SA is effective for use in patients undergoing
elective lumbar laminectomy and/or diskectomy spinal surgery, and was shown to
be the more expedient anesthetic choice in the perioperative setting.
Keywords: spinal anesthesia, general anesthesia,
efficiency, expedient