109229
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

伴有或不伴有肺气肿病变的 COPD 患者中吸气量对呼吸困难评价的作用:一项试验性研究
Authors Cui L, Ji X, Xie M, Dou S, Wang W, Xiao W
Received 17 May 2017
Accepted for publication 1 August 2017
Published 30 September 2017 Volume 2017:12 Pages 2823—2830
DOI https://doi.org/10.2147/COPD.S142016
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Charles Downs
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Background: Since forced expiratory volume in 1 second (FEV1) shows a weak correlation with patients’ symptoms
in COPD, some volume parameters may better reflect the change in dyspnea
symptoms after treatment. In this article, we investigated the role of
inspiratory capacity (IC) on dyspnea evaluation among COPD patients with or
without emphysematous lesions.
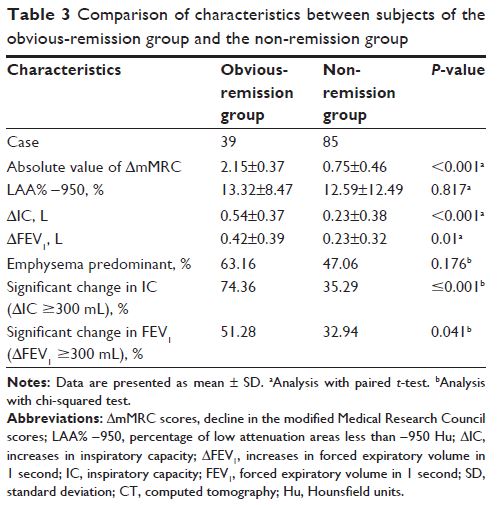
Methods: In this prospective study, 124 patients with
stable COPD were recruited. During the baseline visit, patients performed
pulmonary function tests and dyspnea evaluation using the modified Medical
Research Council (mMRC) scale. Partial patients underwent quantitative
computerized tomography scans under physicians’ recommendations, and
emphysematous changes were assessed using the emphysema index (EI; low
attenuation area [LAA]% −950). These subjects were then divided into the
emphysema-predominant group (LAA% −950≥9.9%) and the non-emphysema-predominant
group (LAA% −950<9.9%). After treatment for ~1 month, subjects returned
for reevaluation of both pulmonary function parameters and dyspnea severity.
Correlation analysis between the change in IC (∆IC) and dyspnea (∆mMRC) was
performed.
Results: Correlation analysis revealed that ∆IC was
negatively correlated with ∆mMRC (correlation coefficient [cc], −0.490, P <0.001) in the total study
population, which was stronger than that between ∆FEV1 and ∆mMRC (cc, −0.305, P =0.001). Patients with absolute
∆mMRC >1 were more likely to exhibit a marked increase in IC
(≥300 mL) than those with absolute ∆mMRC ≤1 (74.36% versus
35.29%; odds ratio [OR], 5.317; P <0.001).
In the emphysema-predominant group, only ∆IC strongly correlated with
∆mMRC (cc, −0.459, P =0.005), while ∆FEV1 did not (P >0.05).
Conclusion: IC could serve as an effective complement to FEV1 in COPD patients undergoing dyspnea evaluation
after treatment. For COPD patients with predominant emphysematous lesions, an
increase in IC is particularly more suitable for explaining dyspnea relief than
FEV1.
Keywords: IC, COPD, mMRC
score, quantitative computerized tomography, emphysema index