108384
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

史蒂文斯—约翰逊综合征与毒性表皮溶解症:来自中华人民共和国的一项 7 年的研究
Authors Sun J, Liu J, Gong QL, Ding GZ, Ma LW, Zhang LC, Lu Y
Published Date December 2014 Volume 2014:8 Pages 2539—2547
DOI http://dx.doi.org/10.2147/DDDT.S71736
Received 25 July 2014, Accepted 27 August 2014, Published 12 December 2014
Background: Stevens–Johnson Syndrome (SJS) and toxic epidermal necrolysis (TEN) are rare
but severe cutaneous drug reactions. They are differentiated based on the
fraction of the body surface area affected. Optimal therapy for SJS and TEN is
a controversial issue.
Objective: We compared the
treatments given to and the clinical outcomes of 39 cases of SJS and 48 cases
of TEN seen at a single institution between January 2007 and December 2013 for
better understanding of the clinical characteristics and development of the two
conditions.
Methods: Demographic data,
clinical characteristics, treatments given, and therapeutic responses observed
were retrospectively collected.
Results: The incidence rates of
hypoproteinemia and secondary infections are significantly higher in TEN than
in SJS (P =0.001 and P =0.002, respectively). The corticosteroid
dose did not influence the time from the initiation of therapy to control of
the lesions in SJS, but increasing the dosage of corticosteroids progressively
decreased the time from the initiation of therapy to control of the lesions in
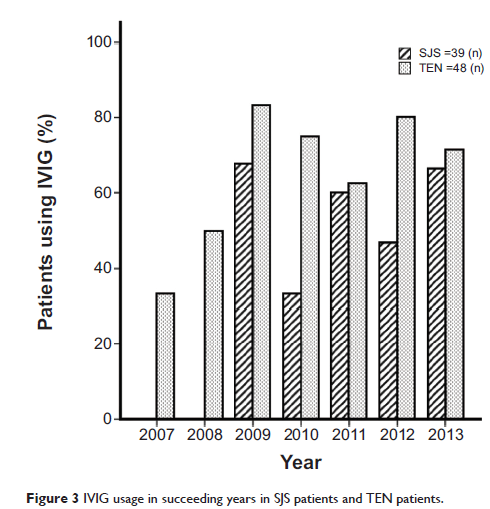
TEN. With increases in the utilization ratio of intravenous immunoglobulin
(IVIG), the length of the hospital stay became shorter, whereas the time from
the initiation of therapy to control of the lesions remained the same in SJS.
However, for TEN, both the length of the hospital stay and the time from the
initiation of therapy to control of the lesions became shorter with increases
in the utilization ratio of IVIG.
Conclusion: SJS and TEN are two
variants of the same spectrum, and they differ from each other not only in the
severity of epidermal detachment but also in other clinical parameters and
their distinct clinical courses. Thus, differential treatment of both
conditions may have benefits for their prognosis.
Keywords: corticosteroids,
intravenous immunoglobulin, Stevens–Johnson Syndrome, toxic epidermal
necrolysis, cutaneous drug reaction