109451
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

复杂区域疼痛综合征 I 型 (CRPS-I) 小鼠的性别差异
Authors Tang C, Li J, Tai WL, Yao WF, Zhao B, Hong J, Shi S, Wang S, Xia Z
Received 11 April 2017
Accepted for publication 10 July 2017
Published 31 July 2017 Volume 2017:10 Pages 1811—1819
DOI https://doi.org/10.2147/JPR.S139365
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 3
Editor who approved publication: Dr Katherine Hanlon
Background: Sex
differences have been increasingly highlighted in complex regional pain
syndrome (CRPS) in clinical practice. In CRPS type I (CRPS-I), although
inflammation and oxidative stress have been implicated in its pathogenesis,
whether pain behavior and the underlying mechanism are sex-specific is unclear.
In the present study, we sought to explore whether sex differences have an
impact on inflammation, oxidative stress, and pain sensitivity in CRPS-I.
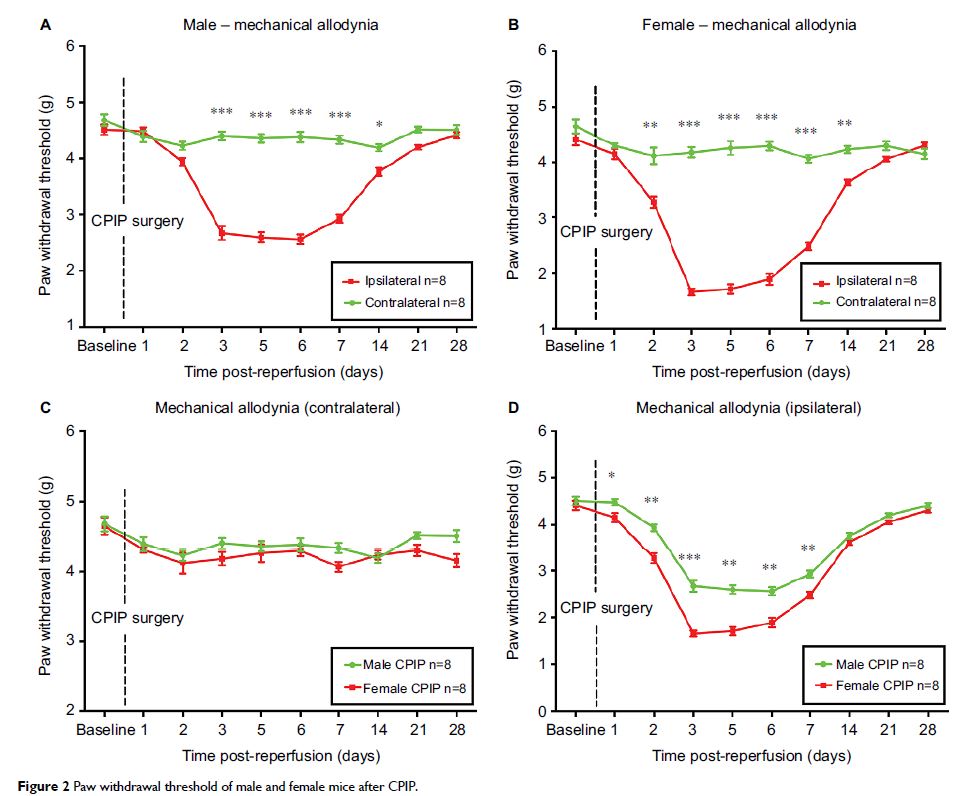
Methods: Chronic post-ischemia pain (CPIP) was established in both male and
female mice as an animal model of CRPS-I. Edema and mechanical allodynia of
bilateral hind paws were assessed after reperfusion. Blood samples were
analyzed for serum levels of oxidative stress markers and inflammatory
cytokines.
Results: Both male and female mice developed edema. Male mice developed
CPIP at day 3 after reperfusion; female mice developed CPIP at day 2 after
reperfusion. Female mice displayed significantly earlier and higher mechanical
allodynia in the ischemic hind paw, which was associated with higher serum
levels of IL-2, TNF-α, isoprostanes, 8 OhdG, and malondialdehyde at day 2 after
reperfusion. Moreover, female mice showed significantly lower SOD and IL-4
compared to male mice at day 2 after reperfusion.
Conclusion: Our results indicate that sex differences in inflammatory and
oxidative stress states may play a central role in the sex-specific nociceptive
hypersensitivity in CRPS-I, and offer a new insight into pharmacology
treatments to improve pain management with CRPS.
Keywords: sex differences, complex regional pain syndrome, chronic
post-ischemia pain, inflammatory response, oxidative stress