109451
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Retrospective study to identify trigeminal–cervical ocular referred pain as a new causative entity of ocular pain
Authors Tseng SC, Cheng AM, Fu Y
Received 2 May 2017
Accepted for publication 9 June 2017
Published 25 July 2017 Volume 2017:10 Pages 1747—1754
DOI https://doi.org/10.2147/JPR.S140895
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Purpose: To
determine the prevalence and clinical characteristics of trigeminal–cervical
(TC) ocular referred pain.
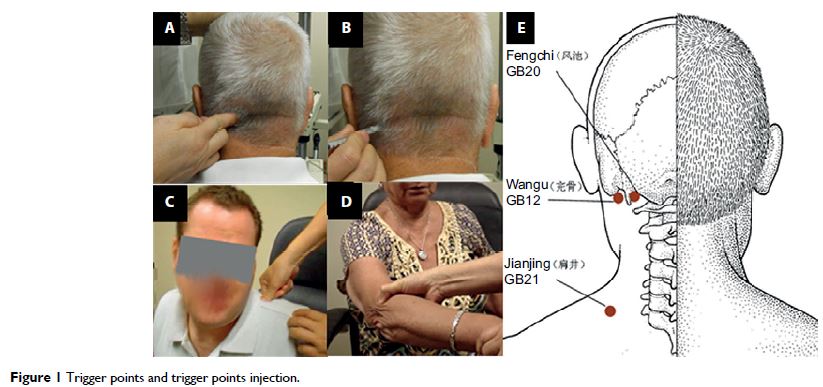
Methods: A retrospective study of 1,680 patients seen during 2002–2010 was
performed in an ocular surface specialty center to identify patients with or
without TC pain defined as ocular pain with ipsilateral trigger points located
at the occipital region. Patients with refractory TC pain despite topical
anesthetics and conventional treatments received interventional injection to
each trigger point.
Results: A total of 81 (4.8%) patients (study group) with TC pain and 241
patients (control group) without TC pain were identified out of the 1,680
patients over an 8 year period. There was no difference in age, gender, prior
surgeries, medications, non-pain symptoms, pain laterality, and concomitant
ocular diseases between the 2 groups. Multivariate regression analysis showed
that patients with TC pain had a significant correlation with persistent deep
ocular pain, ipsilateral trigger points (f 2=99, p <0.001) but not headaches (f 2=0.09, p =0.5). Injection
at the trigger points achieved complete or partial pain resolution with a low
recurrence rate in 43 of 45 (96%) patients with TC pain.
Conclusion: TC pain defined herein may be a different entity of ocular pain and can
indeed be differentiated from other ocular pain by the referral character so
that one may avoid mislabeling it as undetermined or as a reason to
unnecessarily overtreat concomitant ocular diseases.
Keywords: headache, new ocular pain, referred pain, trigeminal–cervical,
trigger point, occipital neuralgia