109451
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

IIIB 期或 IV 期非小细胞肺癌 (NSCLC) 患者的免疫抑制状态与临床特征及化疗反应有关联
Authors Wang Y, Hu GF, Wang ZH
Received 6 March 2017
Accepted for publication 16 June 2017
Published 19 July 2017 Volume 2017:10 Pages 3557—3566
DOI https://doi.org/10.2147/OTT.S136259
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Akshita Wason
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Geoffrey Pietersz
Background: Indoleamine 2,3-dioxygenase (IDO) catalyzes the rate-limiting step of
tryptophan (Trp) degradation via the kynurenine (Kyn) pathway, which inhibits
the proliferation of T cells and induces the apoptosis of T cells, leading to
immune tolerance. Therefore, IDO has been considered as the most important
mechanism for tumor cells to escape from immune response. Previous studies
suggested that IDO might be involved in the progression of tumor and resistance
to chemotherapy. Several preclinical and clinical studies have proven that IDO
inhibitors can regulate IDO-mediated tumor immune escape and potentiate the
effect of chemotherapy. Thus, the present study investigated the correlation
between the clinical parameters, responses to chemotherapy, and IDO activity to
provide a theoretical basis for the clinical application of IDO inhibitors to
improve the suppression status and poor prognosis in cancer patients.
Methods: The serum concentrations of Trp and Kyn were measured by
high-performance liquid chromatography in 252 patients with stage IIIB or IV
non-small-cell lung cancer, and 55 healthy controls. The IDO activity was
determined by calculating the serum Kyn-to-Trp (Kyn/Trp) ratio.
Results: The IDO activity was significantly higher in the lung cancer
patients than in the controls (median 0.0389 interquartile range
[0.0178–0.0741] vs 0.0111 [0.0091–0.0133], respectively; P <0.0001). In addition,
patients with adenocarcinoma had higher IDO activity than patients with
nonadenocarcinoma (0.0449 [0.0189–0.0779] vs 0.0245 [0.0155–0.0563],
respectively; P =0.006).
Furthermore, patients with stage IIIB disease had higher IDO activity than
patients with stage IV disease (0.0225 [0.0158–0.0595] vs 0.0445
[0.0190–0.0757], respectively; P =0.012). The most
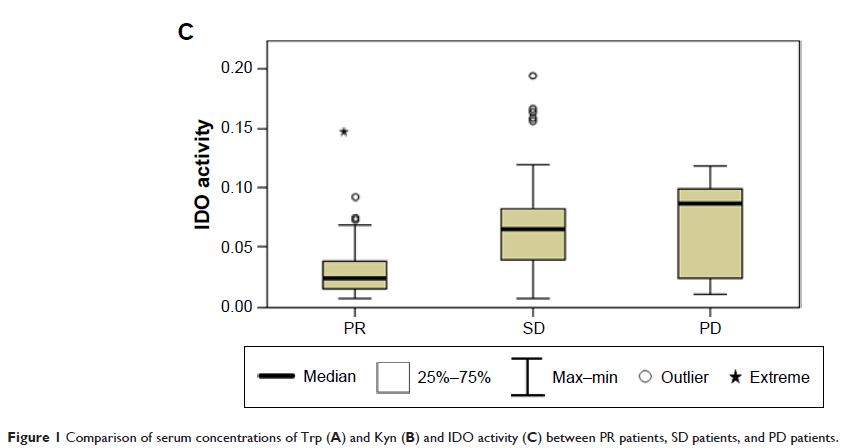
meaningful discovery was that there was a significant difference between the
partial response (PR) patients and the stable disease (SD) and progressive
disease (PD) patients (0.0240 [0.0155–0.0381] vs 0.0652 [0.0390–0.0831] vs
0.0868 [0.0209–0.0993], respectively, P <0.0001).
Conclusion: IDO activity was increased in lung cancer patients. Higher IDO
activity correlated with histological types and disease stages of lung cancer
patients, induced the cancer cells’ resistance to chemotherapy, and decreased
the efficacy of chemotherapy.
Keywords: advanced non-small-cell lung cancer, indoleamine 2,3-dioxygenase,
immune escape, chemotherapy response, tumor immunotherapy