109451
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Cost-utility of collaborative care for the treatment of comorbid major depressive disorder in outpatients with chronic physical conditions. A randomized controlled trial in the general hospital setting (CC-DIM)
Authors Goorden M, van der Feltz-Cornelis CM, van Steenbergen-Weijenburg KM, Horn EK, Beekman ATF, Hakkaart-van Roijen L
Received 6 February 2017
Accepted for publication 11 May 2017
Published 18 July 2017 Volume 2017:13 Pages 1881—1893
DOI https://doi.org/10.2147/NDT.S134008
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Papan Thaipisuttikul
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Purpose: Major depressive disorder (MDD) is highly prevalent in patients
with a chronic physical condition, and this comorbidity has a negative
influence on quality of life, health care costs, self-care, morbidity, and
mortality. Research has shown that collaborative care (CC) may be a
cost-effective treatment. However, its cost-effectiveness in this patient group
has not yet been established. Therefore, the aim of this study was to evaluate
the cost-utility of CC for the treatment of comorbid MDD in chronically ill
patients in the outpatient general hospital setting. The study was conducted
from a health care and societal perspective.
Patients and
methods: In this randomized controlled
trial, 81 patients with moderate-to-severe MDD were included; 42 were randomly
assigned to the CC group and 39 to the care as usual (CAU) group. We applied
the TiC-P, short-form Health-Related Quality of Life questionnaire, and EuroQol
EQ-5D 3 level version, measuring the use of health care, informal care, and
household work, respectively, at baseline and at 3, 6, 9, and 12 months
follow-up.
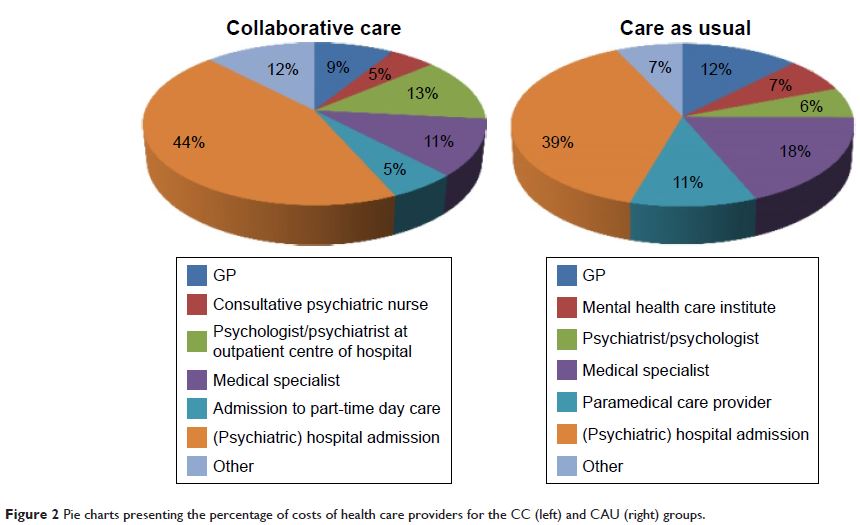
Results: The mean annual direct medical costs in the CC group were €6,718 (95%
confidence interval [CI]: 3,541 to 10,680) compared to €4,582 (95% CI: 2,782 to
6,740) in the CAU group. The average quality-adjusted life years (QALYs) gained
were 0.07 higher in the CC group, indicating that CC is more costly but also
more effective than CAU. From a societal perspective, the incremental
cost-effectiveness ratio was €24,690/QALY.
Conclusion: This first cost-utility analysis in chronically ill patients with
comorbid MDD shows that CC may be a cost-effective treatment depending on
willingness-to-pay levels. Nevertheless, the low utility scores emphasize the
need for further research to improve the cost-effectiveness of CC in this
highly prevalent and costly group of patients.
Keywords: collaborative care, randomized controlled trial, chronic physical
condition, major depressive disorder, cost-utility, general hospital, CC–DIM