109451
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

检查淋巴结数量对子宫颈鳞状细胞癌和腺癌存活率的影响
Authors Zhou J, Zhang WW, Wu SG, He ZY, Sun JY, Wang Y, Chen QH
Received 8 May 2017
Accepted for publication 14 June 2017
Published 18 July 2017 Volume 2017:9 Pages 315—322
DOI https://doi.org/10.2147/CMAR.S141335
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Akshita Wason
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Alexandra Fernandes
Introduction: The
prognostic impact of the number of examined lymph nodes (ELNs) in different
histological subtypes of cervical cancer remains unclear. We aimed to assess
the impact of the number of ELNs in stage IA2–IIA cervical cancer with
different histological subtypes.
Methods: Data of patients with stage IA2–IIA squamous cell carcinoma (SCC)
and adenocarcinoma (AC) of the uterine cervix between 1988 and 2013 were
retrieved from the Surveillance, Epidemiology, and End Results program.
Univariate and multivariate Cox regression analyses were performed to analyze
the effect of number of ELNs on cause-specific survival (CSS) and overall
survival (OS).
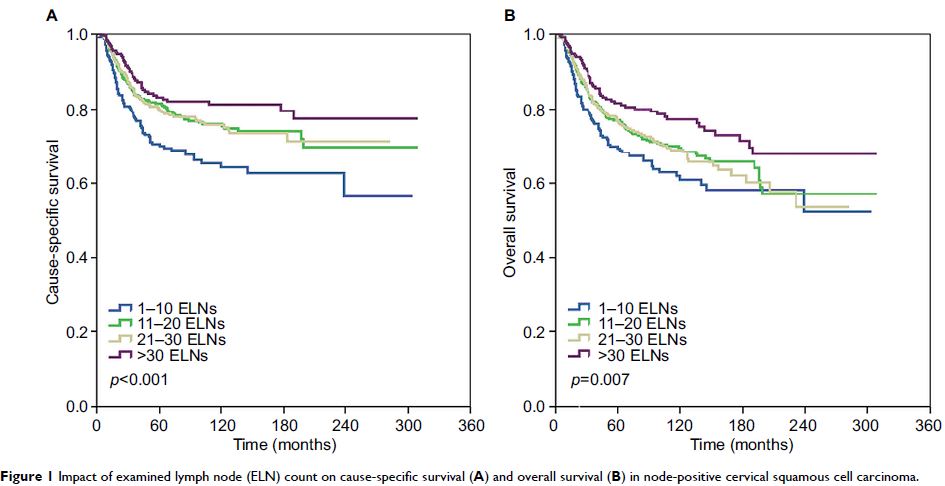
Results: The final data set identified 11,830 patients including 7,920
(66.9%) women with SCC and 3,910 (33.1%) with AC. The median number of ELNs was
19. The multivariate analysis indicated that the number of ELNs was an
independent prognostic factor influencing CSS and OS, both as a continuous or a
categorical variable. Patients with a higher number of ELNs had better survival
outcomes. In SCC subtype, the number of ELNs was also the independent
prognostic factor of CSS and OS in node-positive patients, but not in patients
with node-negative disease. In AC patients, ELN count was not an independent
predictor of CSS and OS regardless of lymph node status.
Conclusion: The number of ELNs is an independent prognostic factor in patients
with stage IA2–IIB cervical cancer. A higher number of ELNs is associated with
better survival outcomes, especially in the node-positive SCC subtype.
Keywords: cervical cancer, early stage, SEER, histological subtype, nodal
positive, prognosis