109568
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

阻塞性睡眠呼吸暂停/呼吸不足综合征患者在鼻腔持续气道正压通气治疗中的依从性对白天嗜睡、疲劳、抑郁和睡眠质量的影响
Authors Wang Y, Ai L, Luo J, Li R, Chai Y, He X, Cao Y, Li Y
Received 20 November 2016
Accepted for publication 28 February 2017
Published 12 April 2017 Volume 2017:11 Pages 769—779
DOI https://doi.org/10.2147/PPA.S128217
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 3
Editor who approved publication: Dr Naifeng Liu
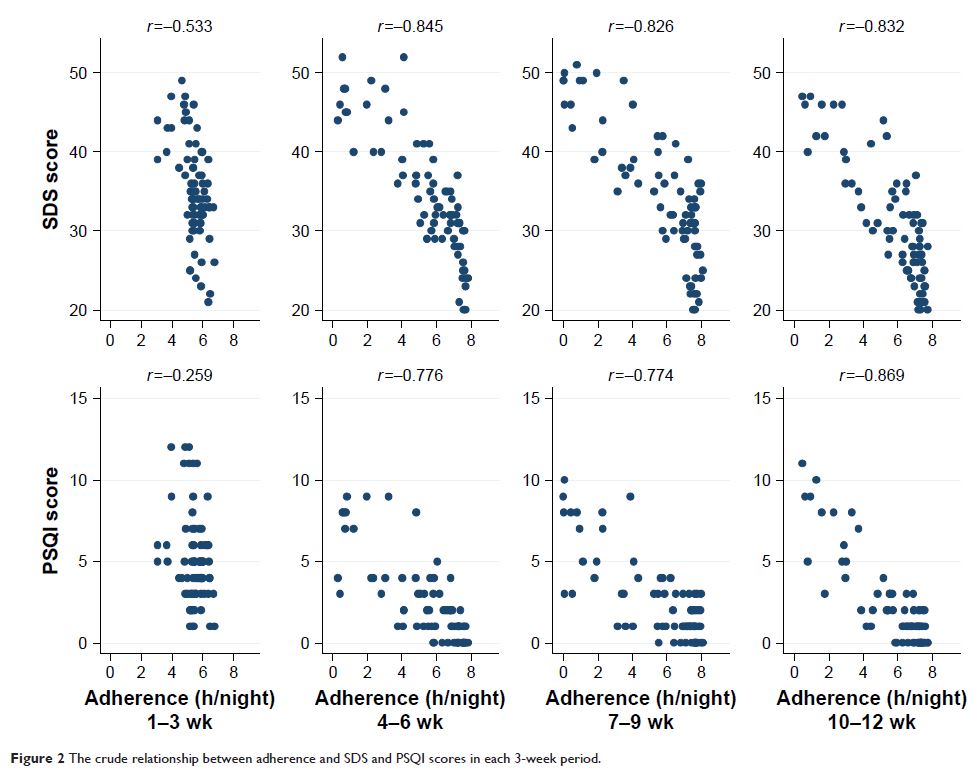
Objectives: The aims of this study were to describe changes in day- and nighttime
symptoms and the adherence to nasal continuous positive airway pressure (nCPAP)
during the first 3-month nCPAP therapy among newly diagnosed patients with
obstructive sleep apnea/hypopnea syndrome (OSAS) and to identify the effect of
adherence on the changes in day- and nighttime symptoms during the first
3 months.
Methods: Newly diagnosed OSAS patients were consecutively recruited from March to
August 2013. Baseline clinical information and measures of the Epworth
Sleepiness Scale (ESS), Fatigue Severity Scale (FSS), Zung’s Self-Rating
Depression Scale (SDS) and the Pittsburgh Sleep Quality Index (PSQI) at
baseline and the end of 3rd, 6th, 9th and 12th week of therapy were collected.
Twelve weeks’ adherence was calculated as the average of each 3-week period.
Mixed model was used to explore the effect of adherence to nCPAP therapy on
ESS, FSS, SDS and PSQI in each 3-week phase.
Results: Seventy-six patients completed the 12-week follow-up. The mixed-effects
models showed that under the control of therapy phase adherence in the range of
<4 hours per night, using nCPAP could independently improve daytime
sleepiness, in terms of ESS (coefficient, [95% confidence interval] unit; –4.49
[–5.62, –3.36]). Adherence at 4–6 hours per night could independently
improve all variables of day- and nighttime symptoms included in this study,
namely ESS –6.69 (–7.40, –5.99), FSS –6.02 (–7.14, –4.91), SDS –2.40
(–2.95, –1.85) and PSQI –0.20 (–0.52, –0.12). Further improvement in symptoms
could be achieved at ≥6 hours per night using nCPAP, which was ESS –8.35
(–9.26, –7.44), FSS –10.30 (–11.78, –8.83), SDS –4.42 (–5.15, –3.68) and PSQI
–0.40 (–0.82, –0.02). The interaction between adherence level and therapy phase
was not significant in day- and nighttime symptoms.
Conclusion: The effect of adherence on the above-mentioned symptoms is stable
through the first 3 months. Under the control of therapy phase, the nCPAP
therapy effectively improves day- and nighttime symptoms with ≥4 hours
adherence, and the patients can achieve a further improvement with
≥6 hours adherence.
Keywords: OSAS, nCPAP, Epworth Sleepiness Scale, Fatigue Severity Scale , Zung’s
Self-Rating Depression Scale, the Pittsburgh Sleep Quality Index