109568
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

超声治疗肌筋膜疼痛综合征的有效性:一个系统评价和综合分析
Authors Xia P, Wang XJ, Lin Q, Cheng K, Li XP
Received 2 January 2017
Accepted for publication 8 February 2017
Published 7 March 2017 Volume 2017:10 Pages 545—555
DOI https://doi.org/10.2147/JPR.S131482
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 4
Editor who approved publication: Dr Katherine Hanlon
Objective: The objective of this review was to assess the therapeutic effect of
ultrasound (US) on myofascial pain syndrome (MPS).
Date sources: PubMed, Embase, and Cochrane Library were searched to
find relevant studies from January 1966 to May 2016 using keywords. Four
investigators performed the data extraction.
Study selection: Randomized controlled trials (RCTs) investigating the
outcomes of pain and physical function between MPS patients receiving and not
receiving US were selected by two researchers independently.
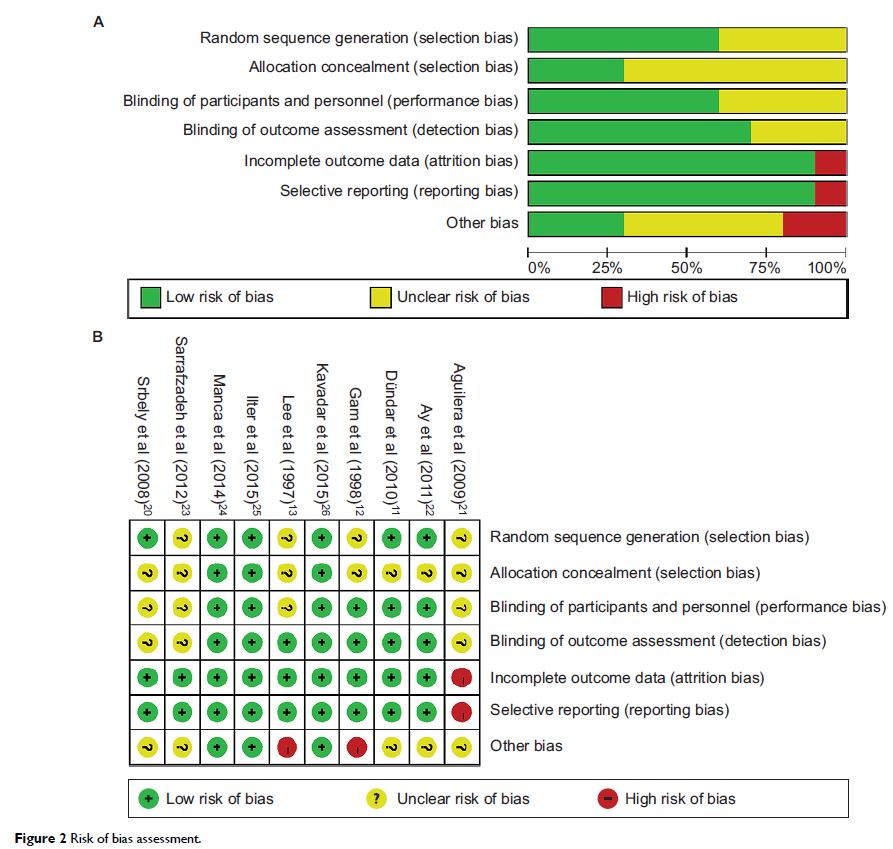
Data extraction: Data were extracted from the RCTs. Risk of bias and
study quality were evaluated following the recommendations of Cochrane
Collaboration. Standardized mean difference (SMD) and 95% confidence interval
(CI) were calculated.
Data synthesis: A total of 10 studies involving 428 MPS patients were
included. US therapy significantly reduced pain intensity (SMD [CI]=−1.41
[−2.15, −0.67], P =0.0002) and increased pain
threshold (SMD [CI]=1.08 [0.55, 1.60], P <0.0001), but had no significant
effect on cervical range of motion (ROM) of lateral flexion (SMD [CI]=0.40
[−0.19, 0.99], P =0.19), rotation (SMD [CI]=0.10
[−0.33, 0.52], P =0.66), or extension or flexion
(SMD [CI]=0.16 [−0.35, 0.68], P =0.53). Heterogeneity between
studies was mainly attributed to differences in the follow-up time, parameter
of US, course of treatment, and the control group. The overall risk of bias
from the included studies was high, and the evidence proving these effect
calculations were assessed as low quality.
Conclusion: Owing to the high risk of bias and the across-trial
heterogeneity of the studies, the current evidence is not clear enough to
support US as an effective method to treat MPS. Clinical trials with
methodological rigorousness and adequate power are needed to confirm it in the
future.
Keywords: ultrasound, myofascial pain syndrome,
meta-analysis