109568
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Evidence of both systemic inflammation and neuroinflammation in fibromyalgia patients, as assessed by a multiplex protein panel applied to the cerebrospinal fluid and to plasma
Authors Bäckryd E, Tanum L, Lind AL, Larsson A, Gordh T
Received 23 November 2016
Accepted for publication 14 December 2016
Published 3 March 2017 Volume 2017:10 Pages 515—525
DOI https://doi.org/10.2147/JPR.S128508
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
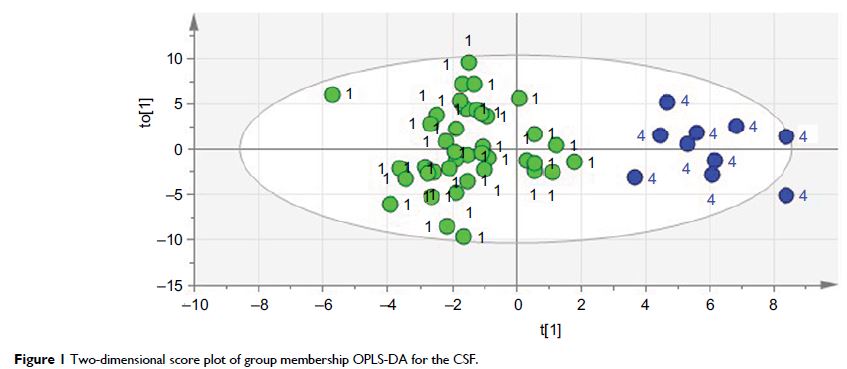
Abstract: In addition to central hyperexcitability and impaired top–down
modulation, chronic inflammation probably plays a role in the pathophysiology
of fibromyalgia (FM). Indeed, on the basis of both animal experiments and human
studies involving the analysis of cytokines and other inflammation-related
proteins in different body fluids, neuroinflammatory mechanisms are considered
to be central to the pathophysiology of many chronic pain conditions. However,
concerning FM, previous human plasma/serum and/or cerebrospinal fluid (CSF)
cytokine studies have looked only at a few predetermined cytokine candidates.
Instead of analyzing only a few substances at a time, we used a new multiplex
protein panel enabling simultaneous analysis of 92 inflammation-related
proteins. Hence, we investigated the CSF and plasma inflammatory profiles of 40
FM patients compared with CSF from healthy controls (n=10) and plasma from
blood donor controls (n=46). Using multivariate data analysis by projection, we
found evidence of both neuroinflammation (as assessed in CSF) and chronic
systemic inflammation (as assessed in plasma). Two groups of proteins (one for
CSF and one for plasma) highly discriminating between patients and controls are
presented. Notably, we found high levels of CSF chemokine CX3CL1 (also known as
fractalkine). In addition, previous findings concerning IL-8 in FM were
replicated, in both CSF and plasma. This is the first time that such an
extensive inflammatory profile has been described for FM patients. Hence, FM
seems to be characterized by objective biochemical alterations, and the
lingering characterization of its mechanisms as essentially idiopathic or even
psychogenic should be seen as definitively outdated.
Keywords: cerebrospinal fluid, chemokines,
chronic pain, cytokines, fibromyalgia, inflammation