109568
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

术前淋巴细胞与单核细胞的比率可预测初级乙肝病毒阳性肝细胞癌后者在治愈性切除后的生存
Authors Li G, Ji J, Yang F, Xu H, Bai Y
Received 12 April 2016
Accepted for publication 23 August 2016
Published 23 February 2017 Volume 2017:10 Pages 1181—1189
DOI https://doi.org/10.2147/OTT.S110411
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Manfred Beleut
Peer reviewer comments 5
Editor who approved publication: Professor Min Li
Background: Both inflammation and immunity are associated with the development of
malignancy. The lymphocyte-to-monocyte ratio (LMR) has been confirmed as a
prognostic factor for several malignant diseases. The purpose of our study was
to analyze prognostic significance of preoperative LMR in hepatitis B virus
(HBV)-related hepatocellular carcinoma after curative resection.
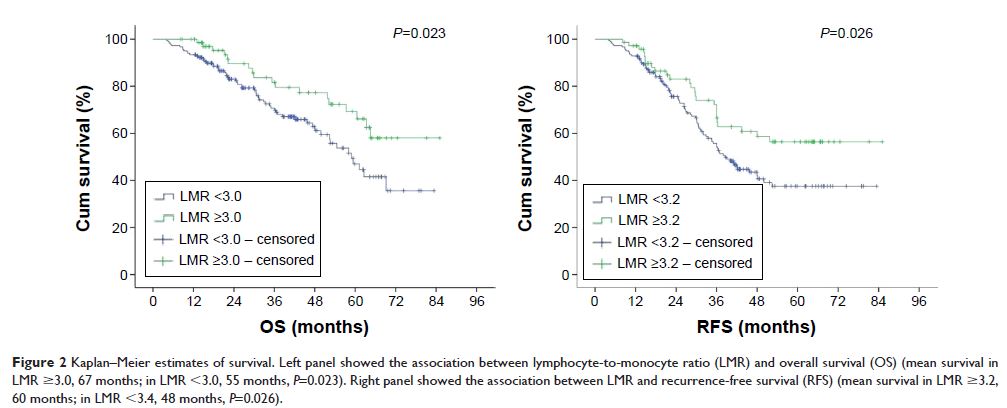
Patients and methods: A total of 253 patients with primary HBV-positive
hepatocellular carcinoma who underwent a curative operation were enrolled in
this retrospective study. The relationship between preoperative LMR and
survival outcomes was analyzed through Kaplan–Meier curves and multivariate Cox
regression analyses.
Results: Patients with a high LMR had a
significantly higher mean overall survival than those with a low LMR (67 months
vs 55 months, P =0.023), and high LMR remained
significant for longer survival in the multivariate analysis (hazard ratio,
0.147; 95% confidence interval [CI]: 0.085–0.253; P =0.021).
Furthermore, patients with a high LMR also had a higher median recurrence-free
survival than those with a low LMR in univariate analyses (60 months vs 48
months, P =0.026) and multivariate analyses
(hazard ratio, 0.317; 95% CI: 0.042–1.023; P =0.032). However, the survival
benefit was limited to patients with advanced cancer.
Conclusion: LMR was confirmed as an independent prognostic
biomarker for primary HBV-positive hepatocellular carcinoma after curative
resection.
Keywords: lymphocyte-to-monocyte ratio,
survival, HBV, hepatocellular carcinoma