109568
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

慢性鼻窦炎与 COPD 患者的支气管扩张患病率和严重程度相关
Authors Yang X, Xu YL, Jin JM, Li RM, Liu XF, Sun YC
Received 9 October 2016
Accepted for publication 16 January 2017
Published 20 February 2017 Volume 2017:12 Pages 655—662
DOI https://doi.org/10.2147/COPD.S124248
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Charles Downs
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Background and
purpose: Bronchiectasis revealed by high-resolution
computed tomography (HRCT) is common in chronic obstructive pulmonary disease
(COPD), but the causes and risk factors remain to be determined. Chronic
rhinosinusitis (CRS) is closely associated with bronchiectasis or COPD, but
whether it is associated with comorbid bronchiectasis in COPD (COPD-Bx) is
unknown.
Patients and methods: Patients with stable COPD were enrolled consecutively
and evaluated for the presence of CRS by questionnaire and paranasal sinus
computed tomography. The presence and severity of bronchiectasis on lung HRCT
were evaluated by the Smith and severity scores. COPD symptoms were evaluated
by COPD Assessment Test (CAT) and Modified British Medical Research Council
Questionnaire. The sputum cell differentials and concentrations of interleukin
(IL)-6, IL-8, IL-5, matrix metalloproteinases-9 (MMP-9), and tissue inhibitor
of matrix metalloproteinases-1 were measured.
Results: We enrolled 136 patients with stable COPD, of which 66
(48.5%) were diagnosed with CRS according to the European Position Paper on
Rhinosinusitis and Nasal Polyps (EP3OS) criteria. The
prevalence of bronchiectasis was 57.6% in patients with CRS, but 37.1% in those
without CRS (P =0.017). COPD-Bx patients with
CRS showed a significantly higher severity score of bronchiectasis than those
without CRS (P =0.034). COPD patients with CRS
had a higher percentage of eosinophils, higher levels of IL-8, IL-6, and MMP-9
in sputum as compared to those without CRS. In COPD-Bx patients with CRS, the
percentage of eosinophils and the levels of IL-6 and MMP-9 in sputum were
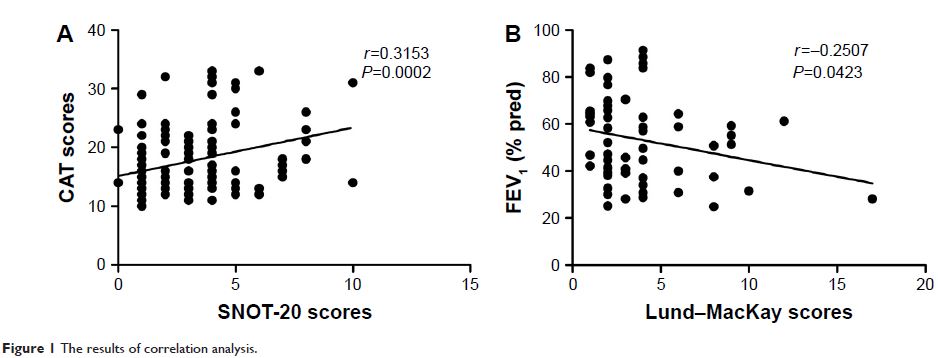
increased as compared to those without CRS. In all the subjects, Sino-Nasal
Outcome Test-20 correlated with CAT score (r =0.315, P <0.01) and in
COPD patients with CRS, Lund–MacKay scores correlated with forced expiratory
volume in 1 s (% pred) (r =−0.251, P <0.05).
Conclusions: CRS was associated with COPD-Bx and this was probably
due to increased airway inflammation.
Keywords: bronchiectasis,
COPD, chronic rhinosinusitis