109568
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Probiotics improve the efficacy of standard triple therapy in the eradication of Helicobacter pylori : a meta-analysis
Authors Lau CSM, Ward A, Chamberlain RS
Received 22 July 2016
Accepted for publication 9 September 2016
Published 7 December 2016 Volume 2016:9 Pages 275—289
DOI https://doi.org/10.2147/IDR.S117886
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Akshita Wason
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Introduction: Helicobacter
pylori colonization is present in half of the world’s population and can lead
to numerous gastrointestinal diseases if left untreated, including peptic ulcer
disease and gastric cancer. Although concurrent triple therapy remains the
recommended treatment regimen for H. pylori eradication, its success rate and
efficacy have been declining. Recent studies have shown that the addition of
probiotics can significantly increase eradication rates by up to 50%. This
meta-analysis examines the impact of probiotic supplementation on the efficacy
of standard triple therapy in eradicating H. pylori .
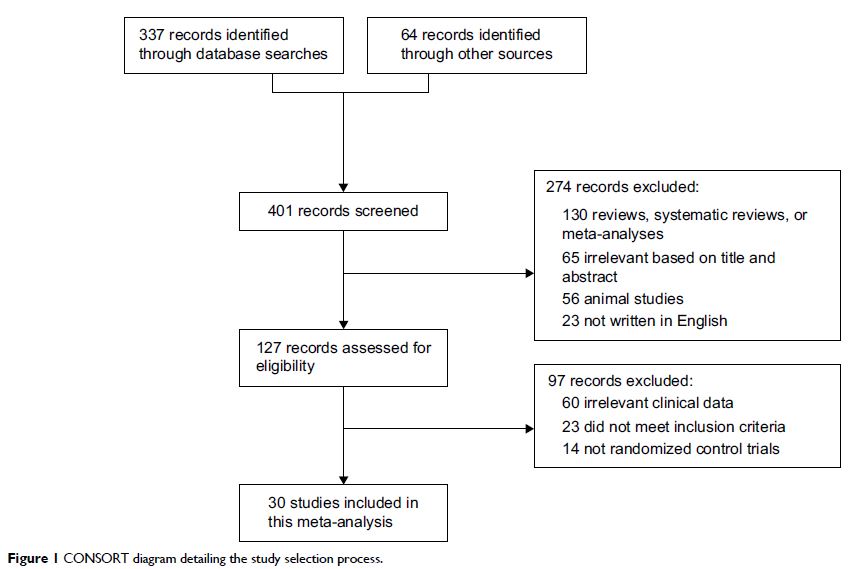
Methods: A comprehensive literature search was conducted using
PubMed, Cochrane Central Registry of Controlled Trials, and Google Scholar
(time of inception to 2016) to identify all published randomized control trials
(RCTs) assessing the use of probiotics in addition to triple therapy for the
treatment of H. pylori . Searches were conducted
using the keywords “probiotics”, “triple therapy”, and “Helicobacter pylori ”. RCTs
comparing the use of probiotics and standard triple therapy with standard
triple therapy alone for any duration in patients of any age diagnosed with H. pylori infection
were included. H. pylori eradication rates (detected using urea
breath test or stool antigen) were analyzed as-per-protocol (APP) and
intention-to-treat (ITT).
Results: A total of 30 RCTs involving 4,302
patients APP and 4,515 patients ITT were analyzed. The addition of probiotics
significantly increased eradication rates by 12.2% (relative risk [RR] =1.122;
95% confidence interval [CI], 1.091–1.153; P <0.001) APP and 14.1% (RR
=1.141; 95% CI, 1.106–1.175; P <0.001) ITT. Probiotics were
beneficial among children and adults, as well as Asians and non-Asians. No
significant difference was observed in efficacy between the various types of
probiotics. The risk of diarrhea, nausea, vomiting, and epigastric pain was
also reduced.
Conclusion: The addition of probiotics is associated with improved H. pylori eradication rates in both children and
adults, as well as Asians and non-Asians. Lactobacillus , Bifidobacterium , Saccharomyces , and
mixtures of probiotics appear beneficial in H. pylori eradication. Furthermore, the
reduction in antibiotic-associated side effects such as nausea, vomiting,
diarrhea, and epigastric pain improves medication tolerance and patient
compliance. Given the consequences associated with chronic H. pylori infection, the addition of probiotics
to the concurrent triple therapy regimen should be considered in all patients
with H.
pylori infection.
However, further studies are required to identify the optimal probiotic species
and dose.
Keywords: probiotics, Helicobacter pylori ,
triple therapy, meta-analysis