109814
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

氯胺酮可增强鼻内右美托咪定诱导的小儿镇静作用:一项随机、双盲试验
Authors Qian B, Zheng W, Shi J, Chen Z, Guo Y, Yao Y
Received 28 June 2020
Accepted for publication 12 August 2020
Published 26 August 2020 Volume 2020:14 Pages 3559—3565
DOI https://doi.org/10.2147/DDDT.S269765
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tuo Deng
Purpose: To compare the efficacy of intranasal dexmedetomidine and dexmedetomidine-ketamine premedication in preschool children undergoing tonsillectomy.
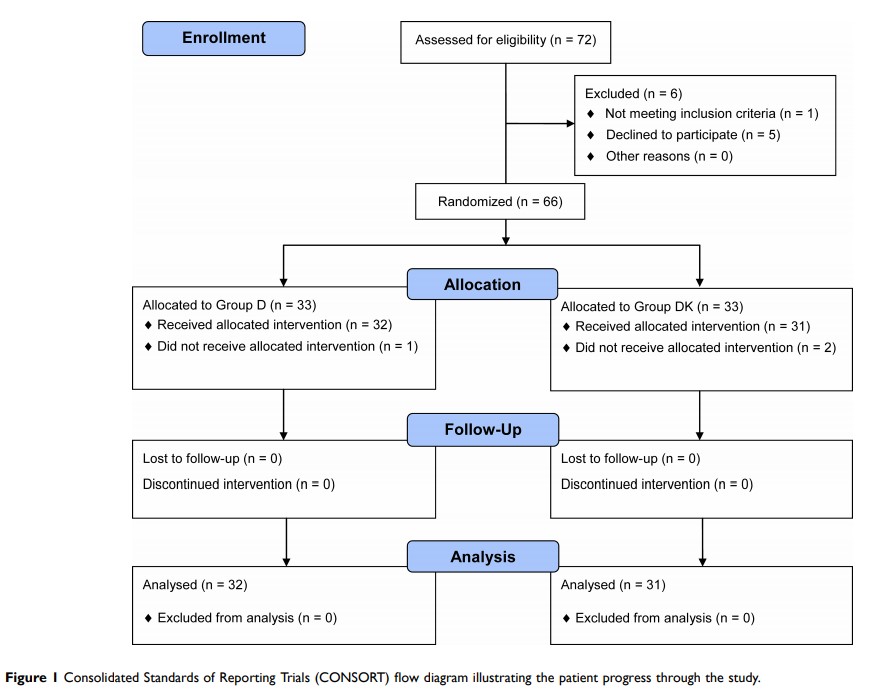
Patients and Methods: We enrolled 66 children with American Society of Anesthesiologists physical status I or II, aged 3– 7 years undergoing tonsillectomy. Patients were randomly allocated to receive intranasal premedication with either dexmedetomidine 2 μg kg− 1 (Group D) or dexmedetomidine 2 μg kg− 1 and ketamine 2 mg kg− 1 (Group DK). The primary outcome was the sedation level assessed by the Modified Observer’s Assessment of Alertness/Sedation Scale (MOAA/S) 30 min after intervention. The minimal clinically relevant difference in the MOAA/S score was 0.5. Secondary outcomes included sedation onset time, parental separation anxiety, acceptance of mask induction, emergence time, emergence delirium, postoperative pain intensity, length of stay in the post-anesthesia care unit (PACU), and adverse effects.
Results: At 30 min after premedication, the MOAA/S score was lower in Group DK than in Group D patients (median: 1.0, interquartile range [IQR]: 1.0– 2.0 vs median: 3.0, IQR: 2.0– 3.0; P < 0.001), with a median difference of 1.0 (95% confidence interval [CI]: 1.0– 2.0, P < 0.001). Patients in Group DK showed considerably faster onset of sedation (15 min, 95% CI: 14.2– 15.8 min) than Group D (24 min, 95% CI: 23.2– 24.8 min), with a median difference of 8.0 min (95% CI: 7.0– 9.0 min, P < 0.001). Both parental separation and facemask acceptance scores were lower in Group DK than in Group D patients (P =0.012 and P =0.001, respectively). There was no significant difference in emergence time, incidence of emergence delirium, postoperative pain scores, and length of stay in the PACU between the two groups.
Conclusion: Intranasal premedication with a combination of dexmedetomidine and ketamine produced better sedation for pediatric tonsillectomy than dexmedetomidine alone.
Keywords: preoperative sedation, mask induction, pediatric anesthesia