109669
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

已发表论文
蛋白酪氨酸磷酸酶 SHP-1 通过调节表皮生长因子受体 (EGFR) 和 HER-2 的磷酸化使 EGFR/HER-2 阳性乳腺癌细胞对曲妥珠单抗 (trastuzumab) 变得敏感
Authors Wu YF, Li R, Zhang JY, Wang G, Liu B, Huang XF, Zhang T, Luo RC
Received 4 February 2015
Accepted for publication 2 April 2015
Published 14 September 2015 Volume 2015:8 Pages 2577—2587
DOI http://dx.doi.org/10.2147/OTT.S82225
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Professor Jianmin Xu
Background: Trastuzumab resistance in HER-2 positive breast cancer cells is closely related to overexpression of both epidermal growth factor receptor (EGFR) and human epidermal receptor (HER-2). SHP-1 has been demonstrated to downregulate tyrosine kinase activity including EGFR via its phosphatase function, but its effect on HER-2 activity is still unknown. Here, we examined the hypothesis that SHP-1 enhances the anticancer efficacy of trastuzumab in EGFR/HER-2 positive breast cancer cells through combining dual inhibition of EGFR and HER-2.
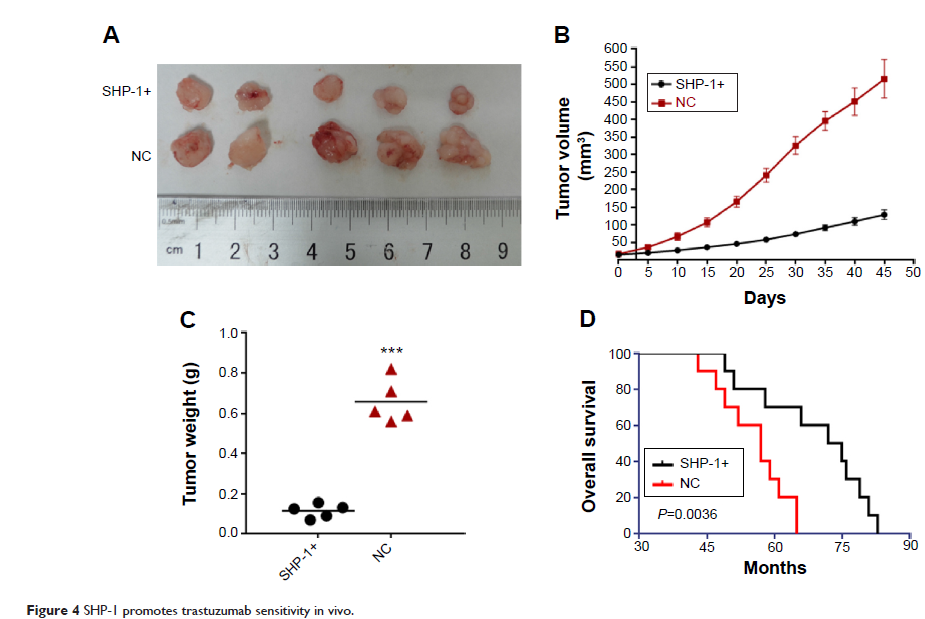
Methods: Trastuzumab-resistant breast cancer SKBr-3 cells were generated by long-term in vitro culture of SKBr-3cells in the presence of trastuzumab. The SHP-1 was ectopically expressed by stable transfection. The activity and expression of EGFR, HER-2, and downstream signaling pathways were tested by Western blot. Cell viability was examined by the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay, and apoptosis was examined by flow cytometry. The binding between SHP-1 and EGFR/HER-2 was evaluated by immunoprecipitation assay and bimolecular fluorescence complementation. The effects of SHP-1 on tumorigenicity and trastuzumab sensitivity were confirmed via in vivo xenograft model.
Results: Trastuzumab-resistant SKBr-3 cells showed aberrant co-expression of EGFR and HER-2. Introduction of wild-type SHP-1 inhibited cell proliferation, clone formation, and promoted the apoptosis induced by trastuzumab. Meanwhile, SHP-1 overexpression reduced phosphorylation levels of EGFR and HER-2 both in parental and trastuzumab-resistant SKBr-3 cells. In vivo study showed an increased antitumor effect of trastuzumab in SHP-1 overexpressed xenografts. At last, we discovered that SHP-1 can make complexes with both EGFR and HER-2, and both phospho-EGFR and phosphor-HER-2 levels in wild-type SHP-1 immunoprecipitates were less than those in phosphatase-inactive SHP-1 (C453S) immunoprecipitates, indicating that EGFR and HER-2 are potential substrates of SHP-1.
Conclusion: Taken together, we have demonstrated that the SHP-1 is a negative regulatory factor of the tyrosine kinase activity of HER-2 and EGFR through inhibiting phosphorylation. Dual targeting of EGFR and HER-2, by combining trastuzumab with SHP-1 overexpression, may improve response in HER-2 overexpressing breast cancer cells that also express high levels of EGFR.
Keywords: breast cancer,trastuzumab, EGFR, HER-2, SHP-1, drug resistance
Methods: Trastuzumab-resistant breast cancer SKBr-3 cells were generated by long-term in vitro culture of SKBr-3cells in the presence of trastuzumab. The SHP-1 was ectopically expressed by stable transfection. The activity and expression of EGFR, HER-2, and downstream signaling pathways were tested by Western blot. Cell viability was examined by the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay, and apoptosis was examined by flow cytometry. The binding between SHP-1 and EGFR/HER-2 was evaluated by immunoprecipitation assay and bimolecular fluorescence complementation. The effects of SHP-1 on tumorigenicity and trastuzumab sensitivity were confirmed via in vivo xenograft model.
Results: Trastuzumab-resistant SKBr-3 cells showed aberrant co-expression of EGFR and HER-2. Introduction of wild-type SHP-1 inhibited cell proliferation, clone formation, and promoted the apoptosis induced by trastuzumab. Meanwhile, SHP-1 overexpression reduced phosphorylation levels of EGFR and HER-2 both in parental and trastuzumab-resistant SKBr-3 cells. In vivo study showed an increased antitumor effect of trastuzumab in SHP-1 overexpressed xenografts. At last, we discovered that SHP-1 can make complexes with both EGFR and HER-2, and both phospho-EGFR and phosphor-HER-2 levels in wild-type SHP-1 immunoprecipitates were less than those in phosphatase-inactive SHP-1 (C453S) immunoprecipitates, indicating that EGFR and HER-2 are potential substrates of SHP-1.
Conclusion: Taken together, we have demonstrated that the SHP-1 is a negative regulatory factor of the tyrosine kinase activity of HER-2 and EGFR through inhibiting phosphorylation. Dual targeting of EGFR and HER-2, by combining trastuzumab with SHP-1 overexpression, may improve response in HER-2 overexpressing breast cancer cells that also express high levels of EGFR.
Keywords: breast cancer,trastuzumab, EGFR, HER-2, SHP-1, drug resistance